COVID-19 Statement from SPROUTING HEALTH CHIROPRACTIC
A Message from Our Practice
We hope that you and your family are well in these unprecedented times.
In keeping with the Australian Government Department of Health recommendations, chiropractors (and other allied health professionals), have been asked to remain OPEN, so that we can continue to support the function and mobility of our patients, and reduce any future stress on GP and emergency services at this time.
Due to the continued updates with the COVID-19 virus, we are urging all patients to please self isolate if they are feeling unwell, so that we do not put other patients, our staff or practitioners at risk of infection.
We need to do all that we can to reduce the transmission of the virus. We are using the highest standards of hygiene, social distancing and screening in the practice.
If you are feeling unwell or have recently travelled overseas, please let us know and we can easily change your appointment. We are implementing the advice from the Australian Government Department of Health as it's updated.
Some things will be different: You will notice that when you make an appointment there will be extra questions asked on the phone, when you arrive at the practice on the door before you can enter, and also at the reception desk to screen potential COVID-19 cases.
You will also notice that our reception chairs are more spaced out to ensure social distancing and we are implementing very strict hygiene measures. We are also limited as to how many people can enter the practice at one time.
In the clinic, we have introduced additional cleaning, strict hand sanitising and alcohol based cleaning for all our reception staff and practitioners to use in between each patient visit, and ask that all patients wash hands or use hand sanitiser at the reception desk when they enter the practice. We have stepped up our usual cleaning practices by also disinfecting all surfaces and door handles constantly.
In the study, “Social Isolation: A Predictor of Mortality Comparable to Traditional Clinical Risk Factors,” (5) researchers found that social isolation predicted mortality for both genders, and that social isolation was as strong a factor in their mortality risk as smoking, and even higher than having high blood pressure. Loneliness and social isolation have the same cardiovascular effects as smoking 15 cigarettes per day, but these factors also increase the risk of “all-cause morbidity,” in other words, dying from any cause. Loneliness increases the risk of developing dementia by 50% and stroke by 32% while increasing the morbidity risk of cancer by 25% (6). Make sure you are dealing with your stress, stay connected to as many people as you can (via phone, internet and following social isolation rules).
Our main priority is the health of our patients so if there is anything we can do to help you or your family in this time please get in contact with us. Please phone us if you need advice or want to ask any questions.
In keeping with the Australian Government Department of Health recommendations, chiropractors (and other allied health professionals), have been asked to remain OPEN, so that we can continue to support the function and mobility of our patients, and reduce any future stress on GP and emergency services at this time.
Due to the continued updates with the COVID-19 virus, we are urging all patients to please self isolate if they are feeling unwell, so that we do not put other patients, our staff or practitioners at risk of infection.
We need to do all that we can to reduce the transmission of the virus. We are using the highest standards of hygiene, social distancing and screening in the practice.
If you are feeling unwell or have recently travelled overseas, please let us know and we can easily change your appointment. We are implementing the advice from the Australian Government Department of Health as it's updated.
Some things will be different: You will notice that when you make an appointment there will be extra questions asked on the phone, when you arrive at the practice on the door before you can enter, and also at the reception desk to screen potential COVID-19 cases.
You will also notice that our reception chairs are more spaced out to ensure social distancing and we are implementing very strict hygiene measures. We are also limited as to how many people can enter the practice at one time.
In the clinic, we have introduced additional cleaning, strict hand sanitising and alcohol based cleaning for all our reception staff and practitioners to use in between each patient visit, and ask that all patients wash hands or use hand sanitiser at the reception desk when they enter the practice. We have stepped up our usual cleaning practices by also disinfecting all surfaces and door handles constantly.
In the study, “Social Isolation: A Predictor of Mortality Comparable to Traditional Clinical Risk Factors,” (5) researchers found that social isolation predicted mortality for both genders, and that social isolation was as strong a factor in their mortality risk as smoking, and even higher than having high blood pressure. Loneliness and social isolation have the same cardiovascular effects as smoking 15 cigarettes per day, but these factors also increase the risk of “all-cause morbidity,” in other words, dying from any cause. Loneliness increases the risk of developing dementia by 50% and stroke by 32% while increasing the morbidity risk of cancer by 25% (6). Make sure you are dealing with your stress, stay connected to as many people as you can (via phone, internet and following social isolation rules).
Our main priority is the health of our patients so if there is anything we can do to help you or your family in this time please get in contact with us. Please phone us if you need advice or want to ask any questions.
Detailed Information about Coronavirus Disease
In December 2019, an outbreak of a novel coronavirus occurred in Wuhan, Hubei Province, China. According to the WHO, the declaration of a pandemic is linked to concerns about COVID-19's spread around the world, rather than changes in the characteristics of the disease (2).
What is the incubation period? - The incubation period is the duration between exposure to the virus and the onset of symptoms. The World Health Organization (WHO) currently estimates that the incubation period ranges from 1 to 14 days, with a median incubation period of 5 to 6 days, this is still being further studied.
How Infectious Is the Virus? The disease is spreading rapidly because it is a novel (new) virus that our bodies have not been exposed to before, our immune system develops immunity by exposure. The reproductive rate of the virus, or R0, measures the average number of secondary infections caused by a single case. Ie how many people are infected from one person on average. The WHO initially estimated the R0 to be 1.4-2.5 (average 1.95), however a recent review of 12 studies estimated the basic R0 to be 3.28 and the median R0 to be 2.79. This is still under investigation.
What is the severity of the disease? In China, the case fatality rate (CFR) is reported to be 2.3%, however this is much higher in Hubei Province (2.9%) than in all other provinces (0.4%). The CFR is likely to be much lower than reported, due to a proportion of mild cases going underreported in the community. CFR estimates for regions outside mainland China are generally low; however, the clinical outcomes for the majority of these cases is still unknown. Based on current estimates, it is estimated that approximately 1% of COVID-19 patients will die. This will be better estimated once serological studies are performed.
Likewise, information is still being gathered on the overall severity of the disease. Based on current data, it is estimated that approximately 80% of cases will have a mild illness, approximately 20% will require hospitalisation, and approximately 3-5% will require ICU admission. Cases classified as critical (respiratory failure, septic shock, and/or multi-organ failure) have a CFR of approximately 50%. Patients in this circumstance have tended to be elderly with comorbidities.
What are the symptoms of COVID-19?
The most common symptoms are fever, tiredness, and dry cough. Some patients may have aches and pains, nasal congestion, runny nose, sore throat or diarrhea. These symptoms are usually mild and begin gradually. Some people become infected but don’t develop any symptoms and don't feel unwell. Most people (about 80%) recover from the disease without needing special treatment. Around 1 out of every 6 people who gets COVID-19 becomes seriously ill and develops difficulty breathing. Older people, and those with underlying medical problems (particularly high blood pressure, heart disease, diabetes, chronic respiratory disease and cancer) are more likely to develop serious illness. About 2% of people with the disease have died. People with fever, cough and difficulty breathing should seek medical attention.
Lets put this all into perspective:
Although 2019-nCoV can cause a severe respiratory illness like severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), evidence from clinics suggested that 2019-nCoV is generally less pathogenic than SARS-CoV, and much less than MERS-CoV (4). 2019-nCoV is the third coronavirus to cross species to infect human populations (probably transmitted from bats or another host) in the past two decades. The previous two are the severe acute respiratory syndrome coronavirus (SARS-CoV) outbreak in 2002 and the Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in 2012.
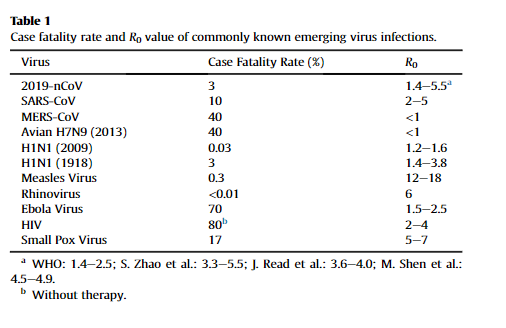
Of the first 41 cases of laboratory confirmed infections with 2019-nCoV, all had viral pneumonia and almost a third of the patients developed acute respiratory distress syndrome (ARDS) requiring intensive care and 6 patients (14.6%) died. Since the fatality rate of the early reported case is often high due to bias towards more severe cases, the true mortality risk might be much lower. As of Jan 27, 2020, when this data was analysed (3), about 3000 cases were confirmed in China, and cases were also reported in Japan, South Korea, Thailand, Singapore, the United States, and Australia, all of which were exported from China. The total number of deaths from the pneumonia-related disease accounts for less than 3%. In addition, most of those who have died had underlying health conditions such as hypertension, diabetes or cardiovascular disease that compromised their immune systems. Although the fatality rate will continue to change until all infected people recover, it appears that 2019-nCoV is less pathogenic than SARS-CoV (∼10%), and much less than MERS-CoV (∼40%)
Table 1. Below demonstrates the current 2019-nCoV seems to have relatively low pathogenicity and moderate transmissibility. However, more information on the biological and epidemiological features of the virus are urgently needed to further refine the risk assessment and response, which will ultimately benefit the 2019-nCoV control and prevention (3).
What is the incubation period? - The incubation period is the duration between exposure to the virus and the onset of symptoms. The World Health Organization (WHO) currently estimates that the incubation period ranges from 1 to 14 days, with a median incubation period of 5 to 6 days, this is still being further studied.
How Infectious Is the Virus? The disease is spreading rapidly because it is a novel (new) virus that our bodies have not been exposed to before, our immune system develops immunity by exposure. The reproductive rate of the virus, or R0, measures the average number of secondary infections caused by a single case. Ie how many people are infected from one person on average. The WHO initially estimated the R0 to be 1.4-2.5 (average 1.95), however a recent review of 12 studies estimated the basic R0 to be 3.28 and the median R0 to be 2.79. This is still under investigation.
What is the severity of the disease? In China, the case fatality rate (CFR) is reported to be 2.3%, however this is much higher in Hubei Province (2.9%) than in all other provinces (0.4%). The CFR is likely to be much lower than reported, due to a proportion of mild cases going underreported in the community. CFR estimates for regions outside mainland China are generally low; however, the clinical outcomes for the majority of these cases is still unknown. Based on current estimates, it is estimated that approximately 1% of COVID-19 patients will die. This will be better estimated once serological studies are performed.
Likewise, information is still being gathered on the overall severity of the disease. Based on current data, it is estimated that approximately 80% of cases will have a mild illness, approximately 20% will require hospitalisation, and approximately 3-5% will require ICU admission. Cases classified as critical (respiratory failure, septic shock, and/or multi-organ failure) have a CFR of approximately 50%. Patients in this circumstance have tended to be elderly with comorbidities.
What are the symptoms of COVID-19?
The most common symptoms are fever, tiredness, and dry cough. Some patients may have aches and pains, nasal congestion, runny nose, sore throat or diarrhea. These symptoms are usually mild and begin gradually. Some people become infected but don’t develop any symptoms and don't feel unwell. Most people (about 80%) recover from the disease without needing special treatment. Around 1 out of every 6 people who gets COVID-19 becomes seriously ill and develops difficulty breathing. Older people, and those with underlying medical problems (particularly high blood pressure, heart disease, diabetes, chronic respiratory disease and cancer) are more likely to develop serious illness. About 2% of people with the disease have died. People with fever, cough and difficulty breathing should seek medical attention.
Lets put this all into perspective:
Although 2019-nCoV can cause a severe respiratory illness like severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), evidence from clinics suggested that 2019-nCoV is generally less pathogenic than SARS-CoV, and much less than MERS-CoV (4). 2019-nCoV is the third coronavirus to cross species to infect human populations (probably transmitted from bats or another host) in the past two decades. The previous two are the severe acute respiratory syndrome coronavirus (SARS-CoV) outbreak in 2002 and the Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in 2012.
Of the first 41 cases of laboratory confirmed infections with 2019-nCoV, all had viral pneumonia and almost a third of the patients developed acute respiratory distress syndrome (ARDS) requiring intensive care and 6 patients (14.6%) died. Since the fatality rate of the early reported case is often high due to bias towards more severe cases, the true mortality risk might be much lower. As of Jan 27, 2020, when this data was analysed (3), about 3000 cases were confirmed in China, and cases were also reported in Japan, South Korea, Thailand, Singapore, the United States, and Australia, all of which were exported from China. The total number of deaths from the pneumonia-related disease accounts for less than 3%. In addition, most of those who have died had underlying health conditions such as hypertension, diabetes or cardiovascular disease that compromised their immune systems. Although the fatality rate will continue to change until all infected people recover, it appears that 2019-nCoV is less pathogenic than SARS-CoV (∼10%), and much less than MERS-CoV (∼40%)
Table 1. Below demonstrates the current 2019-nCoV seems to have relatively low pathogenicity and moderate transmissibility. However, more information on the biological and epidemiological features of the virus are urgently needed to further refine the risk assessment and response, which will ultimately benefit the 2019-nCoV control and prevention (3).
Latest research suggests that the current 2019-nCoV seems to have relatively low pathogenicity and moderate transmissibility. However, more information on the biological and epidemiological features of the virus are urgently needed to further refine the risk assessment and response, which will ultimately benefit the 2019-nCoV control and prevention. Besides, because that anti-coronaviral drugs are still under development, fear plays a role in the economic and social consequences, which was also a feature of SARS-CoV outbreak. Educating the communities and strengthening public confidence is thus very important!. As long as the transmission of the virus from one person to another could be substantially and consistently interrupted (R < 1), it is entirely possible that the outbreak could be controlled and even eradicated, and this requires the joint efforts of the whole society.
Therefore let’s all follow some simple rules.
Keep the environment clean by following the article referenced here:
https://www.health.gov.au/sites/default/files/documents/2020/03/environmental-cleaning-and-disinfection-principles-for-covid-19.pdf
What other advice should we give you, our patients to deal with COVID-19?
1. Get your information from credible sources. Visit www.health.gov.au or your state or territory public health authority website. 2. We stress the importance of personal hygiene measures: · Avoid touching your face 3 · Wash your hands frequently · Cough and sneeze into a tissue and then dispose of tissues and wash your hands, or cough and sneeze into your elbow if a tissue is not available 4· Stay home if you are sick (3).
For a collection of resources for the general public and industry about coronavirus (COVID-19) visit here: https://www.health.gov.au/resources/collections/novel-coronavirus-2019-ncov-resources
References
- Australian Government Department of Health https://mcusercontent.com/4e9516307bb1e10b680dfa405/files/ffeac5b6-9c5c-4b21-8a6e-e1f578571d37/Coronavirus_Covid_19_Information_for_Clinicians.pdf
- https://www.abc.net.au/news/2020-03-12/coronavirus-is-now-pandemic-so-how-does-that-affect-your-family/12048510
- Information for Clinicians Aus Government Department of Health
- Chen, J., 2020. Pathogenicity and transmissibility of 2019-nCoV—a quick overview and comparison with other emerging viruses. Microbes and infection.
- Matthew Pantell, MD, Social Isolation: A Predictor of Mortality Comparable to Traditional Clinical Risk Factors 2013 Am J Public Health November. [PMC free article]
- Holt-Lunstad, J., Smith, T.B., Baker, M., Harris, T. and Stephenson, D., 2015. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspectives on psychological science, 10(2), pp.227-237.